Baby Delivery Emergency Where to Got in Hospitols
Emergency childbirth is the birth of an babe in places or situations other than what was planned. In most cases the location of childbirth is planned ahead of fourth dimension and may exist at habitation, a hospital, a medical facility or a birthing center. In other situations, the birth occurs on the way to these facilities. Oftentimes, no trained medical personnel are nowadays, other times there may be police or other first responders. Emergency measures for delivery are indicated when childbirth is imminent.[1]
Background [edit]
Each twelvemonth more 250,000 women around the earth die from complications due to childbirth or pregnancy, with bleeding and hypertension as the leading causes.[2] Many of these deaths are preventable by emergency care, which include antibiotics, drugs that stimulate wrinkle of the uterus, anti-seizure drugs, claret transfusion, and delivery of infant with assistance (vacuum or forceps delivery) or C-section.[2]
In 2012, 1.36% of births took place outside of a hospital, and this number has been increasing over the last thirty years.[3] This is likely a combination of more than abode deliveries and deliveries at nascency centers, with 66% occurring at habitation and 29% in birthing centers.[3] In a study of dwelling house deliveries in the U.s.a. and Canada, almost 12% of attempted home deliveries required urgent transport to hospital for more than specialized intendance. Reasons for transfer include failure of labor to progress, maternal exhaustion or need for more than pain medication, or maternal/fetal complications (see beneath).[4]
Preparation [edit]
Pregnant women usually seek medical care throughout pregnancy and plan for the birth of a baby with a healthcare team. In an emergency childbirth state of affairs, it is recommended to seek further education and brand a plan.[5]
Early preparation [edit]
Many childbirth education classes cover emergency nascence procedures. Parents are trained to larn the signs of early labor or other indications that may require assistance. Caregivers can take a class on baby and kid life support. Some recommend having a kit of emergency supplies in the home such as: clean towels, sheets, make clean scissors, sterile gloves, germ-free pads, diapers, and instructions for baby-rescue breathing.[6] [7]
Tardily preparation [edit]
Boosted aid may be found by calling 911 (in the U.s.a.) or an applicable number to get emergency medical services or nearby medical staff.[8]
A vehicle driven safely toward medical intendance may be considered an acceptable selection during the starting time phase of labor (dilation and effacement). During the second phase of labor (pushing and birth), a vehicle is usually stopped unless imminently arriving at a medical facility. If a vehicle is taken, additional occupants tin support the mother and babe should assist in delivery. The mother and infant are kept warm throughout.[9]
If unable to reach a medical facility, a safe edifice with walls and a roof are sought that will provide protection from the environment. A warm and dry surface area with a bed is preferable.[10]
Supplies are collected for both the female parent and the babe. Possible supplies may include blankets, pillows, towels, warm clean h2o, warm h2o bottles, soap, clean towels, babe clothes, sheets, sterile gloves, germ-free pads, diapers, identification tags for female parent and baby, and instructions for infant-rescue breathing.[6] [seven] [10] A bed may exist prepared for the baby with a basket or box lined with a blanket or sheets.[10] Items are needed to clamp or tie the umbilical cord in 2 places. Shoestrings or strips of a sheet folded into narrow bands may exist used.[10] These items can be sterilized by boiling (20 minutes) or soaking in alcohol (upward to 3 hours).[10] Scissors or a knife are needed to cut the umbilical string and may be sterilized with the same procedure.[x]
Evaluation [edit]
A background obstetric history should be obtained: how many prior births has the patient had (if this is not her first nascency, the patient'south labor could be short), how many weeks forth is she or what is her estimated date of commitment, any special concerns related to this pregnancy such as beingness told she has twins, being told she has a complication, or even if she has received regular prenatal care. Whatsoever other relevant medical history, allergies, drugs, recent signs of infections (fever) should be asked.[4]
Signs and symptoms [edit]
- Any gush of fluid? This would indicate that the rupture of membranes has occurred releasing amniotic fluid and that labor will probably begin soon if the patient is virtually term.[4] [11]
- Whatsoever vaginal bleeding? Could signal a encarmine evidence, a small amount of bloody belch prior to labor, or if large amounts of bleeding occurred information technology could bespeak potentially life-threatening complications.[4]
- How frequent are her contractions? One mutual recommendation is the patient may be in active labor if contractions are v minutes apart for 1 hour (if rupture of membranes has not occurred).[4] [11]
- Does she feel the urge to push with her contractions? This is an indication commitment volition occur soon.[viii]
Physical exam [edit]
If time permits and if trained: one should obtain vital signs to include maternal heart rate, respiratory charge per unit, blood pressure, temperature, and oxygen rate.[4]
The patient should be draped with available blankets for privacy.
The patient's abdomen should be examined and felt for the presence of contractions,[4] and the intensity, frequency, and length of contractions should be noted.[eleven]
With the patient's permission and privacy, an test of the pelvic surface area should be performed; in general, one would:
- Inspect to meet if there is any presenting part of the baby. The baby's head volition feel hard versus their buttocks volition feel soft.[8]
- If the baby's caput is presenting out of the vagina (crowning), and then delivery will be happening soon and preparation should begin to deliver the baby[eight]
- Trained physicians would behave a manual cervical examination to determine the patient's cervical dilation.
Later the concrete exam and if the patient is not crowning, the patient should be placed in the left lateral decubitus position (laying on her left side).[four]
Delivery of term baby in normal position [edit]
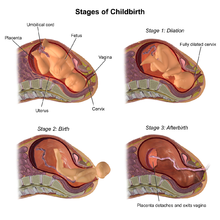
First stage of labor: dilation and effacement of the cervix [edit]
This stage of labor may last from 2 to 18 hours.[12] Further care may be sought during this time.
- Evaluation (in a higher place) is repeated, assessing for alter in stage of labor.[13] [12]
- The mother is encouraged to walk or sit in a comfortable position.[eleven] [13] [12]
Second stage: cervix is dilated [edit]
This stage may last from v minutes to 3 hours.[12]
- Position. The mother is positioned in the lithotomy position, lying on her back, with her anxiety above or at the same level as the hips. The perineum (the space between the vagina and anus) is positioned at the border of a bed.[thirteen] [12]
- Launder. The perineum is cleaned with antiseptic solution or soap and water.[10] Any assistants will wash hands with soap and h2o and put on sterile or make clean gloves.
- Pushing. Pushing is encouraged during contractions.[12] [13]
- Head. The head of the baby is delivered. Delivery of the caput is controlled to foreclose rapid expulsion. Ane mitt is placed on the perineum while the other applies gentle pressure to the baby's head every bit it comes out.[xiii] Soft pressure can be applied to the baby'southward chin through the perineum to assistance expel the caput. Rapid expulsion is still prevented with soft head pressure to reduce vaginal lacerations.[13]
- Cord check. A check is made to look for the presence of an umbilical cord (nuchal cord) around the baby's neck.[12] [thirteen] If it is nowadays, an index finger is used to try to pull information technology over the babe's head.[12] [thirteen] If this cannot be done, the cord is clamped/tied in ii places. So the cord is carefully cut, fugitive injury to the babe or female parent.[12] [13]
- Forepart shoulder. The front shoulder is delivered. This is the shoulder on the mother's front side, towards her belly. The assistant holds the baby's head with ii easily and may need to utilise slight downward force per unit area (towards her anus) to help the forepart shoulder out. Firm force per unit area can injure the babe.[12] [13] If the shoulder gets stuck this is called shoulder dystocia. See procedure for relief of shoulder dystocia (below).
- Back shoulder. The dorsum shoulder is and so delivered by providing slight upward pressure (away from her anus).[13]
- Grab baby. The baby usually comes out right away after both shoulders.[13] The babe is defenseless noting that babies are slippery. The assistant holds the infant at the level of the vagina.
- Cut cord. The umbilical cord is clamped and cut. The cord is clamped in two places about half dozen cm to 8 cm from the baby.[13] The clamps or ties are tight in order to stop the blood flow. The cord is cut betwixt the 2 clamps or ties.[thirteen] [12] Sterilized scissors or a sterilized knife is used.[x] Another banana may aid with this.
- Dry out baby. The babe is dried, wrapped, and kept warm. Advisable neonatal care is provided or the baby is placed to the female parent's breast on her bare pare.[five] An identification ring may exist placed on the baby.[10]
Third stage of labor: the delivery of the placenta [edit]
The baby is attached to the placenta past the umbilical cord. Subsequently the cord is cut, the placenta is normally nonetheless inside the mother. The placenta usually comes out in 2–10 minutes, but information technology may take upwardly to 60 minutes.[x] [12]
- Before the placenta is delivered at that place is a gush of claret as the cord gets longer.[13] [12]
- The umbilical cord tin be held taut, merely must not exist pulled with much force.[13]
- The placenta is delivered and is inspected for completeness. The placenta should be stored in a bag for inspection by trained medical personnel.[xiii] [10]
- The mother will need to have a trained physician inspect for vaginal lacerations that volition demand suture repair.
Maternal complications [edit]
Complications of emergency childbirth include the complications that occur during normal childbirth. Maternal complications include perineal vehement during delivery, excessive haemorrhage (postpartum hemorrhage), retained products of formulation in the uterus, hypertension, and seizures.
Vaginal bleeding and shock [edit]
In a pregnant woman, 40% of the circulating blood volume is in the uterus. This creates a large haemorrhage potential and high take chances of hemorrhagic daze (depression blood force per unit area from loss of circulating blood). For this reason, constant vigilance is important if any of the following occur:
- Vaginal bleeding early on or belatedly in pregnancy
- Severe abdominal pain
- Trauma (such as a fall or car accident) while pregnant
- Uncontrolled vaginal bleeding subsequently the baby is delivered
- Inability to remove the entire placenta after the infant is delivered
Get-go trimester haemorrhage [edit]
Causes of vaginal bleeding early in pregnancy include miscarriage (inevitable or incomplete abortion), embryo implantation and growth outside the uterus (ectopic pregnancy), and placenta attachment at the bottom of the uterus over the neck (placenta previa), all of which can cause significant bleeding.
Bleeding after the first trimester and during delivery [edit]
Prior to and during delivery, haemorrhage can besides occur from tears in the cervix, vagina, or perineum, sudden placental disengagement (abruptio placenta) and placental attachment over the cervix (placenta previa), and uterine rupture.
Haemorrhage after commitment (postpartum hemorrhage) [edit]
Later delivery of the baby, a uterus that is non contracting (atonic uterus), ruptured uterus, remaining parts of placenta or baby or infected remaining parts of placenta or baby can cause severe bleeding. Postpartum haemorrhage is usually managed preventatively past massaging the lower belly (fundal massage), which increases contraction of the uterus and stops haemorrhage. Additionally, steady traction is applied to the cord to prevent trauma, cord avulsion (violent of the umbilical cord), uterine inversion, and retained placental products, all of which can increase claret loss and/or the risk of infection.
Postpartum hemorrhage is defined by loss of more than 500 mL blood within 24 hours after delivery. It is difficult to predict with few known risk factors and occurs in 3% of women, leading to ~150,000 annual deaths worldwide.[x] One time uncontrolled bleeding occurs, management tin exist manual (fundal massage from the outside, packing the uterus, tamponading haemorrhage from the inside with balloon or condom catheter), and pharmacological (with oxytocin, ergotamine, misoprostol). Alongside these treatments, daze should be addressed with IV fluids or claret transfusions as discussed beneath.
Astringent blood loss leading to shock [edit]
In daze, you may come across cold clammy skin, pale skin (especially around eyes, mouth, and easily), sweating, anxiousness, and loss of consciousness. You may note a fast heartbeat (110 beats per minute or more), low blood force per unit area (90mmHg systolic or less), and decreased urine output.
The adult female should be laid on her left side, with legs and buttocks elevated to encourage blood flow dorsum to the heart with gravity. If available, 4 fluids (Ringer's lactate or normal saline) should be started with monitoring of her heart rate, blood force per unit area, and appearance. If available, 2 big bore IV catheters (16-guess or largest bachelor) should be used to rapidly infuse 1L in xv–20 minutes, with a goal of giving 2L in the kickoff hour. If unable to start an IV and the woman is able to beverage and is conscious with no recent convulsions, give 300-500 mL of fluid by mouth. If the adult female is unable to drinkable, is unconscious, or has recently had convulsions, fluid can be given rectally with an enema bag or tin. Fill up the enema with 500mL IV fluid, clamp the end of the tube and insert ten cm (3-4inches) into the rectum. If filling an enema, run water slowly or cramping can occur, pushing the water dorsum out.
Convulsions [edit]
Convulsions (Seizures) in pregnancy can be caused past pregnancy specific causes of seizures such as eclampsia and by normal causes of seizures such equally epilepsy. Warning signs that may atomic number 82 to convulsions include pre-eclamsia, which is a condition that pregnant women can get afterward 20 weeks of pregnancy that is characterized by new-onset high claret pressure, headaches, blurry vision, problem breathing from fluid in lungs, protein in urine from kidney failure, and elevated liver enzymes from liver dysfunction, and possibly coagulation defects from platelet dysfunction.
If a pregnant woman begins to have convulsions, additional help and assistance should be sought. I should not restrain the patient, but prevarication her down on her left side and cheque the airway (mouth, olfactory organ, pharynx). Turning the patient on her side decreases take chances of breathing in vomit and spit. If available, magnesium sulfate is the preferred treatment for seizures in significant women, starting with a dose of 4 mg Iv over 5 minutes.[9] A sensation of warmth during infusion is normal, nonetheless, at that place is also a risk of stopping breathing with magnesium sulfate use, which would indicate the dosage is too high. If this occurs, calcium gluconate can exist used to reverse the effects (1g 4 over 10 minutes, oft in solution).[9] In general, brand sure the breathing rate is at to the lowest degree sixteen breaths per infinitesimal and the genu jerk reflex is nonetheless intact before giving more magnesium sulfate. If magnesium sulfate is unavailable, diazepam can exist used to treat convulsions in pregnancy. The kickoff dose, the loading dose, should be ten mg of diazepam Iv given over 2 minutes.[xiv] After this, the loading dose can be repeated. The maintenance dose is xl mg of diazepam in 500mL IV fluids. The amount of diazepam used should never be more than than 100 mg in 24 hours and it should be dosed in order to keep the adult female awake, rousable, and animate rate higher up sixteen breaths per minute[14]
Fetal care [edit]
Almost x% of newborns crave some resuscitative care. Common complications of childbirth that relate to the baby include breech presentation, shoulder dystocia, infection, and umbilical cord wrapped effectually the babe's cervix (nuchal string).
Evaluation [edit]
The newborn is evaluated at i and five minutes after nativity using the Apgar score, which assigns points based on appearance (color), pulse, grimace (cry), activity (muscle tone), and respiration (animate effort), with each component scored from 0 to 2. Scores below 7 generally require farther care (encounter resuscitation beneath).
Routine care [edit]
Later initial evaluation, babies with good Apgar scores are dried and rubbed, any obstruction of breathing is cleared, and they are warmed either with pare-to-pare contact with the female parent or under a rut source.
Complications [edit]
With United States home births as an estimate, neonatal complications are common, with cord wrapped effectually the head 12-37% of the time (nuchal cord), bereft oxygenation (birth asphyxia) 9% of the time, pulselessness six% of the time, and breech presentation iii% of the time[15]
Breech presentation [edit]

Frank Breech Presentation (buttocks first) is the most common type of breech presentation
Normally, the head is the first part of the body to present out of the birth canal. Notwithstanding, other parts such as the buttocks or feet can present offset, which is referred to as breech presentation. Risk for breech presentation may increase with multiple pregnancies (more i baby), when in that location is too trivial or too much fluid in the uterus, or if the uterus is abnormally shaped.[thirteen] Babies in breech presentation can be delivered vaginally depending on the experience of the provider and if the fetus meets specific low risk criteria, however C-section is recommended if available.[16] Ideally, vaginal breech delivery should non be performed without the availability of nearby emergency C-department capabilities and all-encompassing efforts should be made to bring a woman in labor with breech presentation to a infirmary. There are many variations of breech presentations and multiple ways the baby tin can go stuck during commitment. If a breech delivery is occurring, the provider will guide the hips out by giving light, downward traction belongings the pelvis until the scapula is nowadays. Then at the level of the armpits, each shoulder is delivered by rotating the baby as required, and then afterward rotating 180 degrees to deliver the other shoulder. The head is delivered with careful attention to the baby's artillery. The artillery volition be delivered downwardly through the vulva and may have to be gently held downwardly by the provider's fingers.[11]
Pre-term labor [edit]
Incidence of preterm delivery is approximately 12%, and preterm births are a significant contributing crusade of unplanned emergency delivery.[4] Pre-term labor is defined as occurring before 37 weeks, and risks for pre-term labor include pregnancy with multiple fetuses, prior history of premature labor, structural abnormalities of the cervix or uterus, urinary tract, vaginal, or sexually transmitted infections, high blood pressure, drug use, diabetes, blood disorders, or pregnancy occurring less than six months afterward a prior pregnancy.[11] The same principles of term emergency delivery apply to emergency delivery for a preterm fetus, though the baby will be at college risk of other problems such every bit depression nascency weight, trouble breathing, and infections. The newborn will need additional medical care and monitoring after delivery and should exist taken to a hospital providing neonatal care, which may include antibiotics and breathing treatments.[17]
Shoulder dystocia [edit]
In shoulder dystocia, the shoulder is trapped afterwards the head is delivered, preventing commitment of the rest of the baby. The major hazard gene (other than prior history of shoulder dystocia) is the baby beingness besides big (macrosomia), which can result from the mother being obese or gaining too much weight, diabetes, and the pregnancy lasting too long (post-term pregnancy).[13] Shoulder dystocia can pb to further fetal complications such every bit nerve compression and injury at the shoulder (brachial plexus), fracture of the collarbone, and low oxygen for the fetus (whether due to compression of the umbilical cord or due to inability of the infant to breathe). Shoulder dystocia is often signaled past retreat of the head between contractions when information technology has already been delivered ("turtle sign"). Treatment includes the McRoberts maneuver, where the mother flexes her thighs upwards to her stomach with her knees wide autonomously as pressure is practical on her lower belly, and Woods'southward screw maneuver, where the deliverer inserts a paw into the vagina to rotate the fetus.[18] If all maneuvers neglect, then C-section would exist indicated.
Prolapsed string [edit]

A prolapsed cord refers to an umbilical cord that is delivered from the uterus while the baby is still in the uterus and is life-threatening to the baby. Cord prolapse creates a risk of decreased blood flow (and oxygen flow) to the babe as delivery volition cause string compression. Nevertheless, if the cord delivers before the babe, the cord should non be placed back into the uterus through the cervix since this increases chance of infection.[nineteen] Emergent obstetric care for C-section would be indicated, and in the meantime, one should drag the foot of the bed if possible to endeavor to go on the baby above the level of the cord.[4] If no specialized care is available, one may attempt to reduce pressure of the string manually and continue commitment, merely this is frequently difficult to do.
Nuchal cord [edit]
Afterwards the baby crowns, the umbilical cord may be found to be wrapped around the neck or body of the babe, which is known as nuchal string. This is common, occurring in up to 37% of term pregnancies, and most exercise non cause any long-term problems.[xx] This wrapped cord should exist slipped over the head and then it is not pulled during delivery. If the wrap is not removed, it can choke the infant or can crusade the placenta to detach suddenly which tin can cause astringent maternal bleeding and loss of blood and oxygen to the baby. The cord may too be wrapped around a limb in breech presentation, and should similarly be reduced in these cases.
Resuscitation [edit]
If the infant is not doing well on its own, further care may be necessary. Resuscitation typically starts with warming, drying, and stimulating the newborn. If breathing difficulty is noted, the airway is opened and cleared with suction and oxygen is monitored; if necessary, one may consider using a positive airway pressure ventilator (which gives oxygen while keeping the airway open up) or intubation. If the heart rate is below 60 beats per minute, CPR is started at 3:ane compression to ventilation ratio, with compressions given at the lower breastbone. If this fails to revive the newborn, epinephrine will exist given.[four]
Resuscitation is not indicated for newborns below 22 weeks of gestation and weighing below 400 grams. Resuscitation may also be discontinued if the baby'due south heart does not commencement after 10–15 minutes of full resuscitation (including breathing treatments, medications, and CPR).
In civilisation [edit]
The reports of emergency childbirth are typically of general interest. A mobile app was adult in Ethiopia that guides users through the procedures of assisting with an emergency birth.[21]
References [edit]
![]() Using Wikipedia for Research
Using Wikipedia for Research
- ^ "Emergency Childbirth: MedlinePlus Medical Encyclopedia Epitome". medlineplus.gov . Retrieved iii August 2017.
- ^ a b Holmer, H; Oyerinde, Yard; Meara, Jg; Gillies, R; Liljestrand, J; Hagander, 50 (2015-01-01). "The global met demand for emergency obstetric care: a systematic review". BJOG: An International Journal of Obstetrics & Gynaecology. 122 (2): 183–189. doi:10.1111/1471-0528.13230. ISSN 1471-0528. PMID 25546039. S2CID 25934089.
- ^ a b MacDorman, Marian F.; Matthews, T. J.; Declercq, Eugene (March 2014). "Trends in out-of-infirmary births in the United States, 1990-2012". NCHS Information Brief (144): 1–8. ISSN 1941-4927. PMID 24594003.
- ^ a b c d e f g h i j 1000 Frasure, Sarah Elisabeth (2016). "Emergency Delivery". In Tintinalli, Judith E.; Stapczynski, J. Stephan; Ma, O. John; Yealy, Donald M.; Meckler, Garth D.; Cline, David G. (eds.). Tintinalli'south Emergency Medicine: A Comprehensive Written report Guide (8 ed.). New York, NY: McGraw-Hill Education.
- ^ a b Yevich, Steve (2001). Special Operations Forces Medical Handbook. US Authorities. pp. three–87.
- ^ a b "Information for Meaning Women-What You Can Practice". emergency.cdc.gov . Retrieved 3 August 2017.
- ^ a b Publications, Harvard Health (September 2005). "Emergencies and Kickoff Aid - Childbirth - Harvard Health". Retrieved 3 August 2017.
- ^ a b c d "Precipitous nascence not occurring on a labor and delivery unit". uptodate.com . Retrieved 2017-11-26 .
- ^ a b c Blouse, Ann; Gomez, Patricia (2003). Emergency Obstetric Care (PDF). United States Agency forvInternational Evolution.
- ^ a b c d e f chiliad h i j chiliad l Iserson, Kenneth (2016). Improvised Medicine: Providing Care in Extreme Environments, 2e. McGraw-Hill Education. pp. Affiliate 31. ISBN978-0-07-184762-9.
- ^ a b c d e f Cunningham, F. Gary (2013). "Williams Obstetrics, 20-4th Edition". Retrieved 2017-12-01 .
- ^ a b c d eastward f thou h i j thousand l grand Ballad, Archie (2013). CURRENT Diagnosis & Handling: Obstetrics & Gynecology, 11e. The McGraw-Colina Companies. pp. chapter vii. ISBN978-0-07-163856-2.
- ^ a b c d e f g h i j k l m n o p q r s Cunningham, F; et al. (2014). Williams Obstetrics, Twenty-4th Edition. McGraw-Colina Education. ISBN978-0-07-179893-eight.
- ^ a b Us Agency for International Development, Editors: Ann Blouse and Patricia Gomez (Sep 2003). "Emergency Obstetric Care: Quick Reference Guide for Frontline Providers" (PDF). USAID.
- ^ "Obstetrics/Gynecology." 'Improvised Medicine: Providing Care in Extreme Environments, 2e' Ed. Kenneth Five. Iserson. New York, NY: McGraw-Hill, http://accessmedicine.mhmedical.com.ucsf.idm.oclc.org/content.aspx?bookid=1728§ionid=115697898.
- ^ "Manner of Term Singleton Breech Delivery - ACOG". acog.org . Retrieved 2017-12-12 .
- ^ "Preterm Labor - Gynecology and Obstetrics - Merck Manuals Professional person Edition". Merck Manuals Professional person Edition . Retrieved 2017-12-12 .
- ^ "Fetal Dystocia - Gynecology and Obstetrics - Merck Manuals Professional Edition". Merck Manuals Professional Edition . Retrieved 2017-12-12 .
- ^ Kahana, B; Sheiner, E; Levy, A; Lazer, Southward; Mazor, K (2004). "Umbilical cord prolapse and perinatal outcomes". Int J Gynaecol Obstet. 84 (2): 127–32. doi:10.1016/S0020-7292(03)00333-3. PMID 14871514. S2CID 31686188.
- ^ Peesay, Morarji (2012-08-28). "String around the neck syndrome". BMC Pregnancy and Childbirth. 12 (Suppl ane): A6. doi:10.1186/1471-2393-12-S1-A6. ISSN 1471-2393. PMC3428673.
- ^ Kuo, Lily. "A mobile app could make childbirth safer in Ethiopia, one of the deadliest countries to have a babe". Retrieved 3 August 2017.
Source: https://en.wikipedia.org/wiki/Emergency_childbirth
0 Response to "Baby Delivery Emergency Where to Got in Hospitols"
Postar um comentário